
Announcement: Closing operations at the end of September 2023
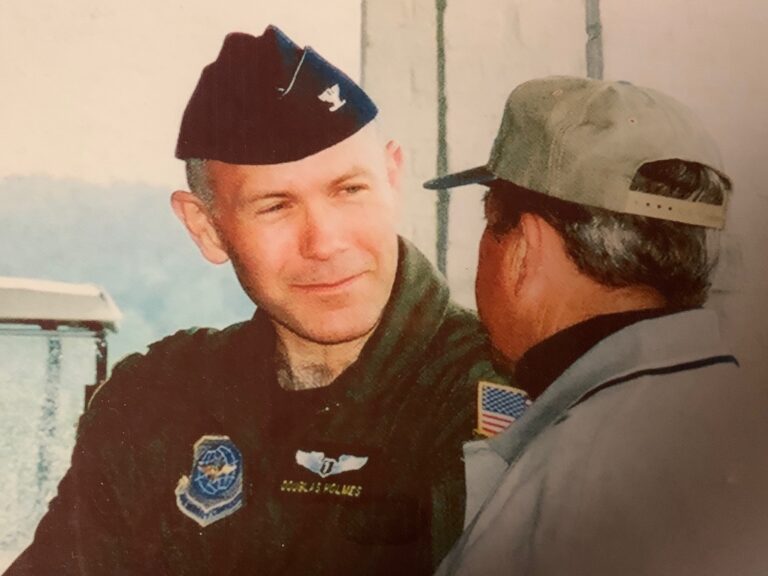
April 4, 2023 For Our Patients and Their Families: After 24 years of private practice, Dr. Holmes has decided to leave a final professional

April 4, 2023 For Our Patients and Their Families: After 24 years of private practice, Dr. Holmes has decided to leave a final professional
Capt Pete Mitchell, USN fighter pilot, call sign “Maverick”, swoops his fighter jet through the valley, crests the mountain top, avoiding setting off the

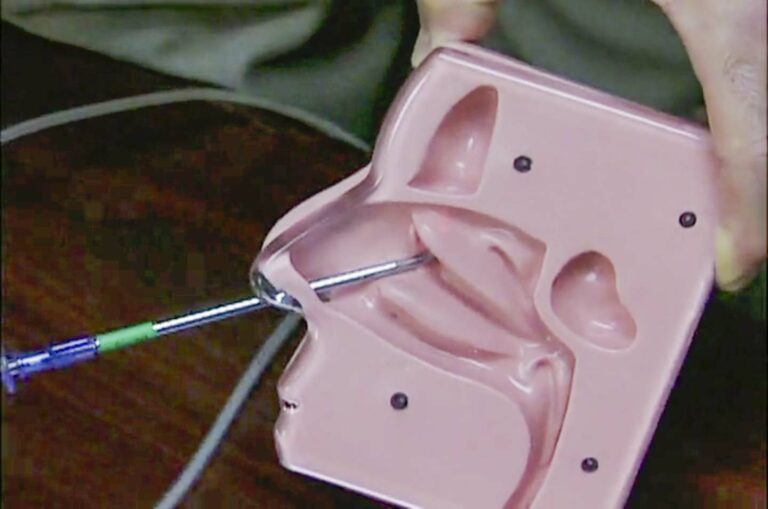
Read more about our journey to offering cochlear implants. We are now proudly offering cochlear implants through our Raleigh, NC office.
When you’ve been in practice for many years,when you have some gray hair,gray being the majority of the hair I have left, and many

I have studied loss and grief just like any other physician, including the classic works of Kubler-Ross’ grief stages of death and dying. All

An open letter to insurance moderators and the medical world, regarding retrograde cricopharyngeus (CP) dysfunction (RCPD), no burpers: Thank you for the opportunity to

I hesitate to add to the cacophony surrounding the corona virus, but these are ‘unprecedented’ times, or so that’s what I’ve heard and read
“You’re a bad ass” he said as I walked into his hospital room, making post op rounds from the previous day’s surgery. Yesterday I

While we are focusing so much attention on the coronavirus, we mustn’t lose focus on our other healthcare needs. The need for my wife
For urgent or compelling needs, our office is open for face-to-face (with a mask), hands-on (with gloves) good old fashioned in-person office visits and
One of the challenges of practicing medicine today is the relative isolation of doctors from other doctors, especially referral sources and recipients of those
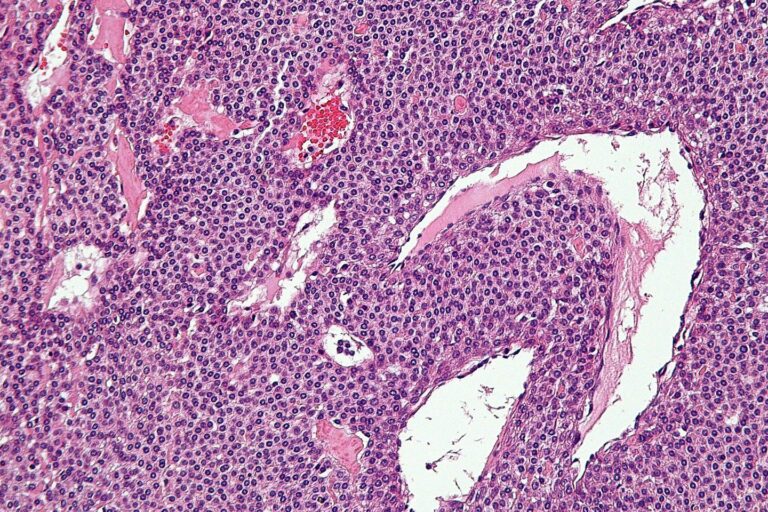
Sinusitis 101 It is uncommon for sinus infections to spread outside of the sinus into the eye or brain, but certainly the possibility exists
In the OR, working through a speculum with an opening the size of a BIC pen, I surgically raised up the right ear drum

Very little is more contentious in medicine than the topic of medical malpractice, lawsuits, and tort reform. The large number of stakeholders with financial and emotional capital are immense.

Severe nosebleeds (epistaxis in medical jargon) are a great example of the secondary, often adverse effects of medical advances which run up the bill for medical costs in the United States. Read on …

If you are lucky, one day you will fall in love. It happens to most all of us at one time or another. It’s actually a psychosis, this falling in love thing. Endorphins bathe our brains with that top of the world, nothing can hurt us euphoria.

When I finished my residency training in 1985, I had the impression that all the great, interesting, challenging cases could be found only at the tertiary care university setting. How wrong I was, how naive I was.

In my life there have been several extraordinary experiences that have led to the creation of the human being that I am. The man that I am. The person that I am. Take note that I have not said the ‘surgeon’ that I am.

I have treated and continue to treat many uninsured patients in my practice. And invariably, when thinking about diagnostic and treatment options for their condition, I come to think how on God’s earth am I able to provide the medical care they need without totally running up a huge bill and huge debt for them!!!

It is certainly no mystery that golf and surgeons go hand in hand. Most surgeons play golf, or at least it seems that way by the animated talk and expressions by those golfing surgeons when the topic arises.

What happens in the OR, or more specifically what happens in my head when an unexpected intraoperative situation dictates a change of direction? It is much better to have considered all the possible scenarios, to have a contingency plan, and to have discussed these plans and possibilities with the patient and family.

I was called out in the middle of my Sunday evening activities for an emergency – bleeding after a tonsillectomy. It is a very scary event to be sitting at home or sleeping about a week after your tonsillectomy, and then suddenly feel a warm liquid in your mouth that you either swallow or let run out, and then look in the mirror or in your hands and discover your own blood.

On this most holy of days, we honor our fathers and forefathers. I had the good fortune of attending church and having brunch with two of my three grown children (the oldest is in Europe pursuing her graduate studies). My resident step son honored me with a beautiful book of a collection of golf photos .
The pressing issue of the day is the shape and form of the upcoming healthcare reform. Unfortunately, none of the current proposals actually reform healthcare. They merely increase the numbers of insured that will be eligible to have their healthcare bills covered by whatever insurance (government sponsored or private plans) these reforms provide.

The trenches, where the real tough, gritty work is done, aptly describes the daily life and work of a community surgeon. ENT (ear, nose, and throat) in my case.